- Welcome to Leenxa
Real Time Insurance Verification, Zero Stress
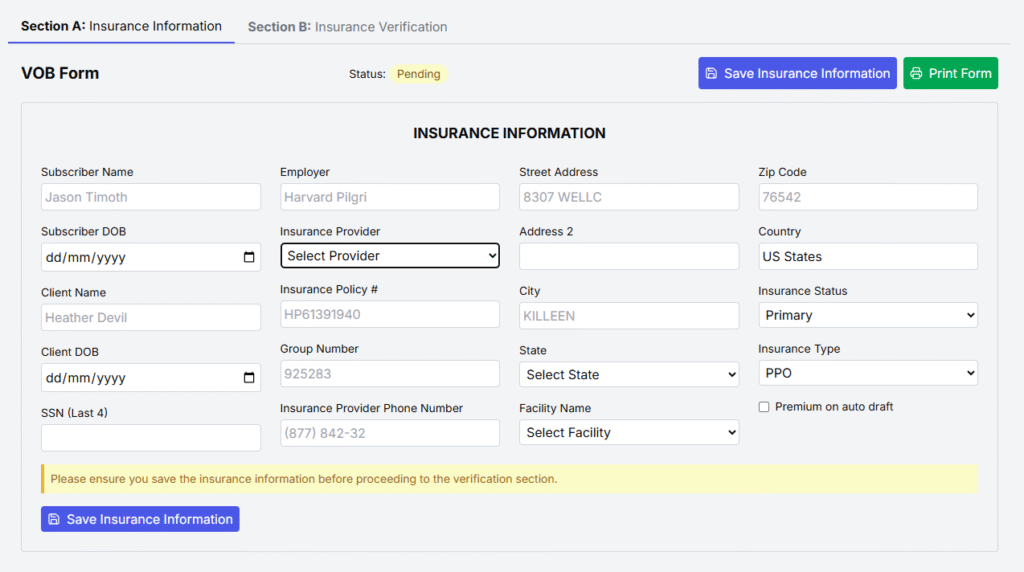
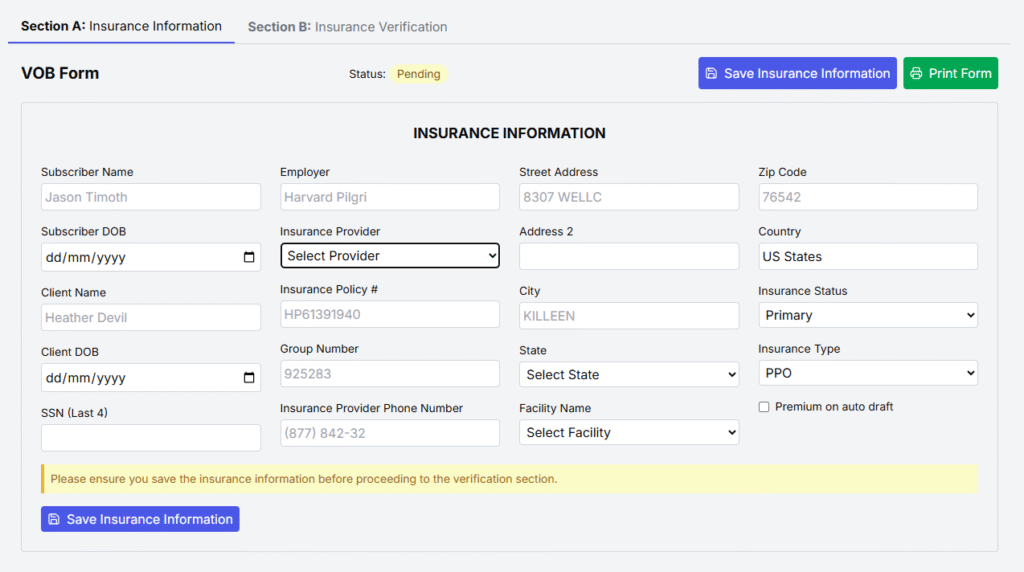
Leenxa removes the guesswork from insurance. In just a few taps, you see eligibility, benefits, copays, and authorization needs all in one simple screen.
- Download on the App Store
Insurance Verification Shouldn’t Be This Hard.
Every day, you lose time, money, and trust not because you deliver poor care, but because insurance answers are slow, unclear, or missing.

Endless Insurance Calls
You spend hours on the phone, waiting on hold, transferring calls, and still walking away unsure about coverage.

Unclear Coverage Details
Deductibles, copays, limits, and exclusions are buried in confusing responses leaving you guessing what’s actually covered.

Denied Claims After Care
You do the work, submit the claim, and then get denied because benefits weren’t verified correctly upfront.

Awkward Patient Conversations
Patients are upset when surprise bills appear and you’re left explaining something you didn’t even know.
Flexible solutions designed to fit your workflow, reduce denials, and strengthen financial performance.
You don’t need more spreadsheets, phone calls, or disconnected tools.
Leenxa gives you a smarter way to verify benefits, understand reimbursement, and make confident decisions all in one place.
Whether you want full automation or simple access to core VOB tools, Leenxa adapts to how your team works today and scales as you grow.
Full Suite Solution
Ideal for providers seeking complete end-to-end solution, analytics, and scalability.
Advanced Repricing Methodology
Perfect for teams that need access to core VOB features. Includes :
- Access to the VOB Questionnaire
- Allowed Amount Calculator
- Raw Reimbursement Data Access
Features
Our Verification of Benefits (VOB) tool is built to do more than just confirm coverage it empowers your entire revenue cycle management process.
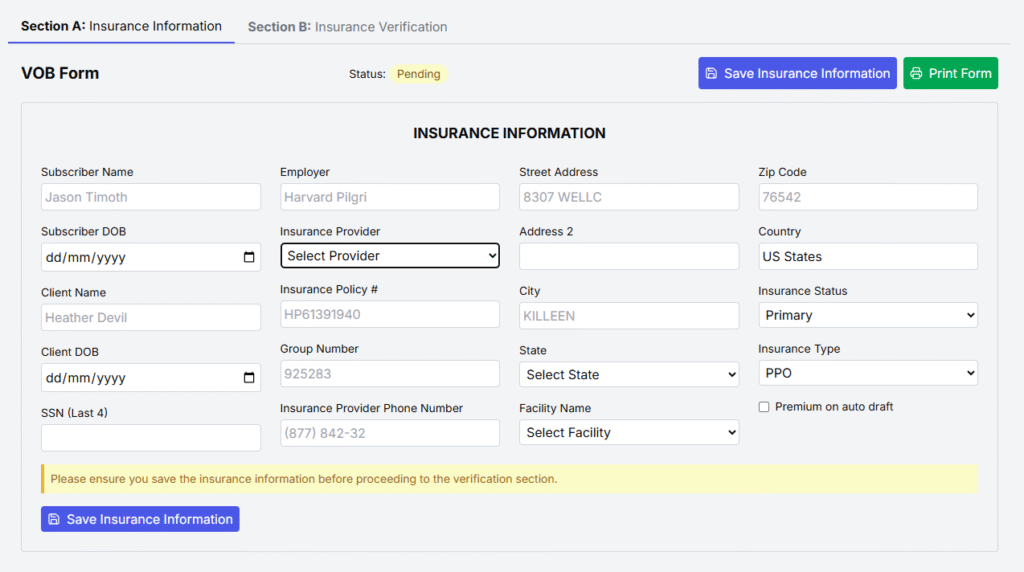
VOB Questionnaire
A dynamic and customizable questionnaire that captures all essential benefit details,…
Repricing Methodology
Quickly identify network status and its financial impact : 1: Historical claims data, 2: Payer-specific fee schedules
In-Network vs. Out-of-Network Insights
Quickly identify network status and its financial impact
See Lynxa in Action
Don’t just take our word for itsee how Lynxa transforms insurance verification in real time.
By watching this demo, you’ll understand exactly how Lynxa simplifies your workflow, improves accuracy, and creates a seamless experience for both providers and patients.
Frequently Asked Questions.
Accuracy is our top priority. Leenxa uses both automation and human verification to ensure you always get reliable results.
Your staff spends hours on calls. Lynxa reduces that to minutes, freeing them for higher-value work.
Not at all. Leenxa is designed to be simple—you’ll be up and running in minutes.
Absolutely. We follow strict healthcare compliance standards to keep all patient data secure.
Yes—Lynxa integrates easily, so you don’t have to change your workflow.
Leenxa is built for all sizes affordable for small clinics, scalable for large hospitals.
Most clients see fewer denials and faster payments within the first 30 days.
Definitely. Patients get clarity on costs upfront, which builds trust and satisfaction.
Our support team is available whenever you need us we’ll never leave you behind.
Lynxa cuts out the waiting, errors, and confusion—giving you instant, accurate answers.
